As we continue to produce these Landmark Newsletters, you may have wondered if we forgot about the controversial therapy lecanemab for patients with early Alzheimer’s disease. Rest assured, we are here to provide “clarity” about this landmark trial.
To review, lecanemab is a humanized monoclonal antibody that binds to soluble amyloid-beta protofibrils associated with Alzheimer’s disease. Given its promising results from a phase 2b trial, the investigators proceeded to conduct the phase 3 trial (Clarity AD).
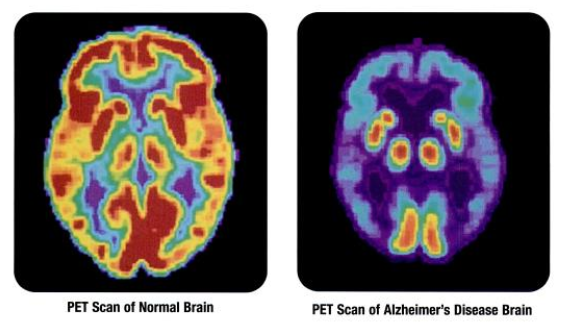
Clarity AD was a double-blind, parallel-group trial that enrolled participants in a 1:1 ratio; patients were assigned to receive either intravenous lecanemab (10 mg/kg every 2 weeks) or placebo. Enrolled participants were between 50 and 90 years of age. Inclusion criteria included a diagnosis of mild cognitive impairment or mild Alzheimer’s disease with evidence of amyloid pathology from PET scan results or CSF analysis. The primary endpoint was the difference in Clinical Dementia Rating–Sum of Boxes (CDR-SB) score after 18 months of treatment.
The trial screened 5,967 individuals, of whom 1,795 underwent randomization. After 18 months of treatment, the adjusted mean change in CDR-SB was 1.21 in the lecanemab group and 1.66 in the placebo group (difference, −0.45; 95% CI, −0.67 to −0.23; P<0.001). Regarding secondary endpoints, patients treated with lecanemab showed a decrease in their mean amyloid level on PET scan (P<0.001). Amyloid-related imaging abnormalities (ARIA) with edema or effusions occurred in 12.6% of the lecanemab group (2.8% were symptomatic) and 1.7% of the placebo group. ARIA with cerebral microhemorrhages, cerebral macrohemorrhages, or superficial siderosis occurred in 17.3% (0.7% were symptomatic) of the lecanemab group and 9.0% of the placebo group.
Based on the results of this study, the FDA approved lecanemab for adult patients with Alzheimer’s disease. However, controversy remains regarding equal access, cost-effectiveness, and adverse events related to ARIA. Salloway et al. (2023) conducted a comprehensive review of ARIA management strategies in anti-amyloid trials, providing valuable insights for clinicians administering lecanemab. Furthermore, a cost-effectiveness analysis by Lin et al. (2023) raised important questions about the economic implications of widespread lecanemab adoption.
To conclude, even though no one is forgetting about this drug anytime soon, we hope this newsletter has provided more clarity about the evidence behind its approval.
- van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in Early Alzheimer’s Disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
- Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412-2414. doi:10.1212/wnl.43.11.2412-a
- Roytman M, Mashriqi F, Al-Tawil K, et al. Amyloid-Related Imaging Abnormalities: An Update. AJR Am J Roentgenol. 2023;220(4):562-574. doi:10.2214/AJR.22.28461
- Swanson CJ, Zhang Y, Dhadda S, et al. Treatment with lecanemab in early Alzheimer’s disease selectively reduces Aβ-associated tau accumulation. Alzheimers Res Ther. 2023;15(1):95. doi:10.1186/s13195-023-01233-6
- Salloway S, Chalkias S, Barkhof F, et al. Amyloid-Related Imaging Abnormalities in 2 Phase 3 Studies Evaluating Lecanemab in Early Alzheimer Disease. JAMA Neurol. 2023;80(2):172-181. doi:10.1001/jamaneurol.2022.4812