Demyelinating diseases such as multiple sclerosis, ADEM, and optic neuritis are a mainstay of neurology, and as such are a very high-yield topic on neurology exams. The RITE® and board examinations ask numerous questions on this topic that command an understanding of diagnostic imaging and pathology as well as therapeutic approaches. Luckily, you will find all of that here! Use this chapter to review the most commonly tested demyelinating diseases, examine real patient pathology and radiology images, and test your retention with our Question Bank and flashcards.
Authors: Ryan Orie PA-C, James Eaton, MD
Editor: Brian Hanrahan MD
Multiple sclerosis (MS)
- Multiple sclerosis is a chronic inflammatory disorder characterized by progressive neurological decline that manifests in different clinical phenotypes.
- Risk factors: Gender (female), family history, geographical latitude, low vitamin D levels.
- Patients can have a broad spectrum of acute focal neurological symptoms including but not limited to focal sensory or motor deficits, monocular visual loss, diplopia, and gait disturbance.
- Patients with chronic MS or other demyelinating conditions tend to have fatigue exacerbated by heat (Uhthoff’s phenomenon) that improves with cooler temperatures.
- Sleep disturbances, depression, euphoria, urinary retention, paroxysmal spasms and cognitive decline are also common.
- Neuropsychological testing can show deficits in long term memory (most common), verbal fluency as well as speed and working memory.
- Epilepsy is a rare complication, seen in only 2-5% of patients.
Diagnosis
- Comprehensive diagnostic criteria are outlined by the 2017 McDonald Criteria.
- Diagnosis is based on patients that have evidence of demyelination with dissemination in space and time.
- This can be based on clinical changes (relapse), features on imaging, and CSF findings.
- Dissemination in space (DIS): Development of lesions in two distinct anatomical locations indicating a multifocal disease process.
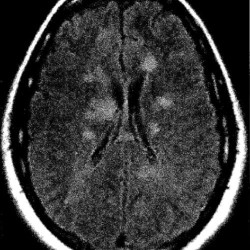
- Dissemination in time (DIT): Appearance of new CNS lesions on imaging over time, or lesions of different appearance (bright versus dark) indicating new and old.
- Oligoclonal bands in CSF are now considered an indication of DIT as well.
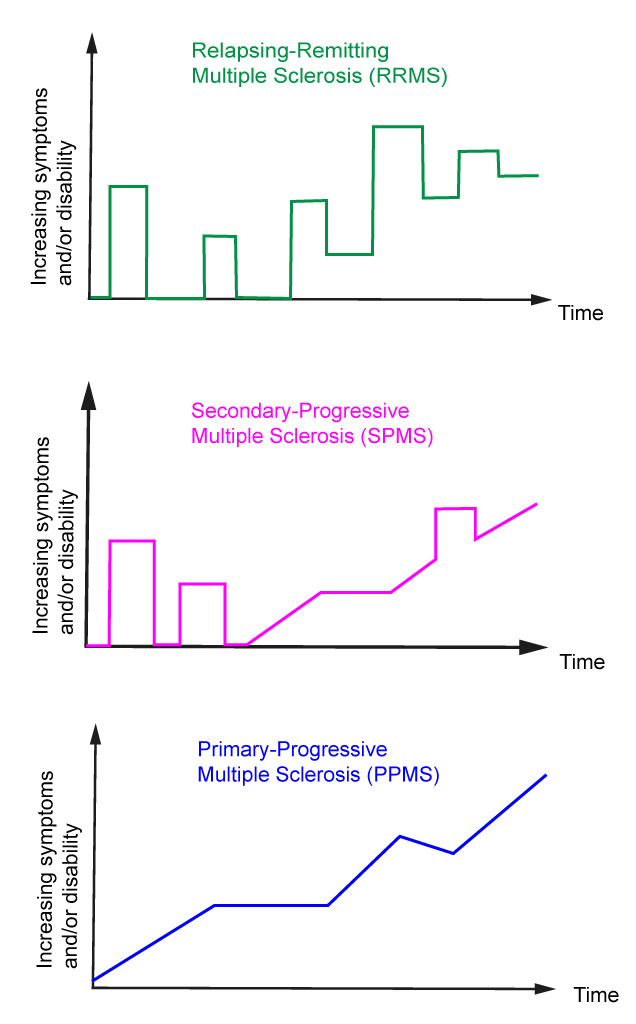
Clinical Phenotypes
- Remitting-relapsing MS (RRMS): Clearly defined attacks with neurologic recovery (complete or incomplete) between them.
- Secondary progressive MS (SPMS): Seen in patients who initially had RRMS but now experiencing a gradual worsening regardless of occasional attacks. Early aggressive treatment may delay this progression.
- Primary progressive MS (PPMS): Progressive decline of neurological function without clearly defined attacks over the course of at least 1 year.
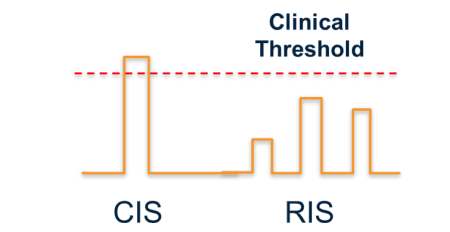
Clinically isolated syndrome (CIS)
- Defined as a monophasic demyelinating episode in someone who otherwise has no clinical history of demyelinating disease.
- Initiating a disease-modifying therapy (DMT) after CIS can delay the time to a definitive diagnosis of multiple sclerosis (MS).
Radiologically isolated syndrome (RIS)
- Diagnosed in a patient with an MRI that is consistent with MS but they have no clinical history of transient focal neurological deficits.
- When diagnosed patients have a 33% chance of having a clinical demyelinating attack over the following two years.
- The risk of MS is higher if oligoclonal bands are present in the CSF.
Diagnostic studies
- Typical findings in CSF include an elevated protein, elevated CSF IgG index, oligoclonal bands in the CSF which do not present in the serum, and possibly slight elevation of WBC count (lymphocytic predominant).
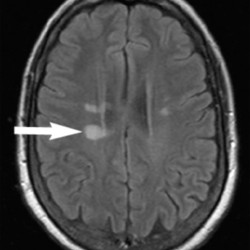
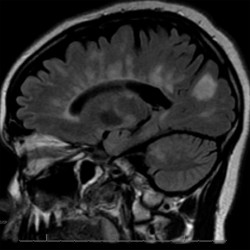
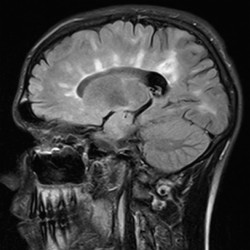
- MRI imaging with contrast is the most important imaging modality in the workup of possible MS.
- Demyelinating lesions related to MS are ovoid, >3 mm in diameter, and are typically located in particular regions: periventricular (Dawson’s fingers), juxtacortical, cortical, or spinal cord.
Typical demyelinating attacks
Optic Neuritis (ON)
- Presents with monocular decreased visual acuity, loss of color vision, and an afferent pupillary defect (APD) due to a demyelinating lesion of the optic nerve.
- Pain is also usually present with extraocular movements.
- Children with ON are more likely to present with headache and bilateral symptoms.
- Can be the initial presentation of multiple sclerosis or neuromyelitis optica.
- A funduscopic exam will show a swollen optic disc.
- Optical coherence tomography (OCT) will show thinning of the retinal nerve fiber layer weeks to months after an acute attack.
- Visual evoked potentials (VEPs) of the affected eye will show a prolonged P100 latency, even in patients with distant histories of ON with no residual visual deficits.
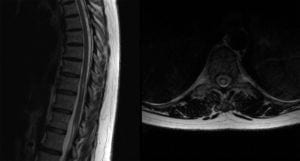
Transverse myelitis (TM)
- Presents with myelopathic findings (weakness, hyperreflexia, sensory symptoms, and occasionally bladder/bowel dysfunction).
- Lhermitte’s sign, an electric shock sensation down the neck/spine with neck flexion or extension) may also be present.
- MRI will show a T2/FLAIR hyperintense lesion involving the spine +/- contrast enhancement based on the lesion’s acuity.
- TM can be the initial presentation of demyelinating disease. However, it is also important to exclude infectious, rheumatologic, postvaccination/postinfectious, and nutritional mimics of demyelinating disease.
- If felt to be truly inflammatory or idiopathic TM once other etiologies are ruled out, then initiation of steroids is indicated.
Log in to View the Remaining 60-90% of Page Content!
New here? Get started!
(Or, click here to learn about our institution/group pricing)1 Month Plan
Full Access Subscription
$142.49
$
94
99
1 Month -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
3 Month Plan
Full Access Subscription
$224.98
$
144
97
3 Months -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
1 Year Plan
Full Access Subscription
$538.47
$
338
98
1 Year -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
Popular
Loading table of contents...
Loading table of contents...